Celiac disease management is a lifelong, multifaceted strategy centered on strict adherence to a gluten-free diet to induce remission and prevent autoimmune damage. This comprehensive guide involves mastering label reading, eliminating cross-contact risks in shared kitchens, navigating social dining scenarios, and maintaining regular medical follow-ups to monitor nutrient absorption and antibody levels.
Receiving a celiac disease diagnosis is a pivotal moment. It transforms food from a simple source of fuel into a daily medical calculation. Unlike dietary fads, celiac disease management requires precision, vigilance, and a robust understanding of how gluten interacts with your immune system and your environment. This guide serves as your “Celiac Compass,” directing you through the complexities of healing your gut and reclaiming your quality of life.
Introduction to Celiac Disease Management
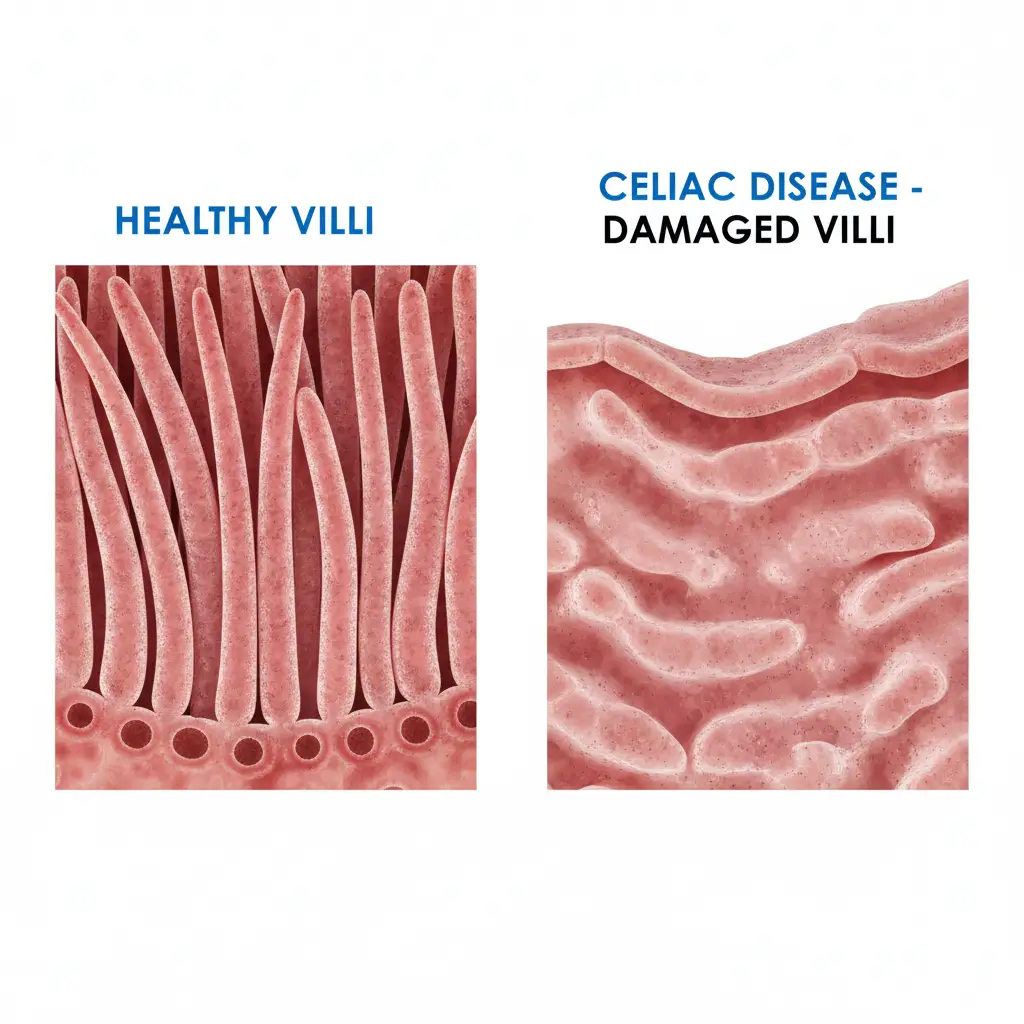
Effective celiac disease management begins with a fundamental shift in perspective: food is your medicine. For the estimated 1% of the global population with this autoimmune disorder, the ingestion of gluten—a protein found in wheat, barley, and rye—triggers an immune response that attacks the small intestine. This damage blunts the villi, the microscopic finger-like projections responsible for nutrient absorption.
Managing this condition is not merely about avoiding bread and pasta; it is about systemic inflammation control. When a patient commits to management, they are committing to the cessation of this autoimmune attack. The goal is mucosal healing, which can take anywhere from six months to two years depending on the severity of the damage and the strictness of the diet.
The Scope of Management
True management extends beyond the dinner plate. It encompasses checking medications for gluten-based fillers, verifying the safety of beauty products (like lip balms that may be ingested), and educating close contacts about the severity of the condition. It is a holistic lifestyle adjustment designed to protect the immune system from accidental exposure.
The Importance of Strict Adherence
One of the most difficult concepts for newly diagnosed patients to grasp is the zero-tolerance policy of the gluten-free diet. In celiac disease management, there is no such thing as “a little bit” of gluten. Research indicates that as little as 10 milligrams of gluten per day—roughly the size of a breadcrumb—can perpetuate intestinal damage in sensitive individuals.
Why “Cheat Days” Are Dangerous
In other dietary frameworks, a cheat day might result in a caloric surplus or temporary bloating. In celiac disease, voluntary ingestion of gluten reactivates the autoimmune process. This can lead to immediate symptoms like gastrointestinal distress, brain fog, and joint pain, but more critically, it increases the long-term risk of complications such as osteoporosis, infertility, and in rare cases, intestinal lymphoma. Strict adherence is the only known method to reduce these risks to that of the general population.
Understanding Cross-Contact
Cross-contact (often mistakenly called cross-contamination) occurs when a gluten-free food comes into contact with gluten, rendering it unsafe. This is the most common reason for persistent symptoms in patients who believe they are following the diet correctly. Common vectors for cross-contact include:
- Shared Toasters: Crumbs from regular bread can stick to gluten-free bread.
- Deep Fryers: Oil used to fry breaded items retains gluten proteins.
- Condiment Jars: Double-dipping a knife spread on wheat toast back into a jar.
- Colanders and Strainers: Gluten creates a sticky residue in mesh that is difficult to remove.

Navigating Medical Challenges
Celiac disease management is not a “diagnose and dismiss” scenario. It requires ongoing medical surveillance to ensure the diet is working and to manage associated risks.
The Follow-Up Schedule
After diagnosis, a robust management plan includes regular check-ups. Typically, gastroenterologists recommend follow-ups at 3 months, 6 months, and then annually. During these visits, physicians monitor tTG-IgA antibody levels. A decline in these antibodies suggests that the gluten-free diet is effective and the autoimmune reaction is subsiding. If levels remain high after a year, it indicates inadvertent gluten exposure.
Nutritional Deficiencies
Because celiac disease damages the upper part of the small intestine where many micronutrients are absorbed, deficiencies are common at diagnosis. Part of your management strategy must include monitoring and replenishing:
- Iron: Anemia is often the primary symptom of celiac disease.
- Vitamin B12 and Folate: Essential for nerve function and energy.
- Vitamin D and Calcium: Critical for bone health, which is often compromised in celiac patients.
Supplementation should always be done under the guidance of a healthcare provider to avoid toxicity and ensure the supplements themselves are gluten-free.
Dietary and Kitchen Safety Protocols
Creating a “safe zone” is vital for mental and physical well-being. For many, the home kitchen is the only place where they can eat without anxiety. Establishing a gluten-free kitchen requires systematic organization.
The Mixed-Household Dilemma
While a 100% gluten-free household is the safest option, it is not always improved for families with non-celiac members. If you must maintain a shared kitchen, strict protocols are necessary:
- Color Coding: Use specific colors (e.g., green stickers or red cookware) for gluten-free items.
- Top-Shelf Rule: Store gluten-free foods on the top shelves of the pantry and refrigerator. Gravity causes crumbs to fall; you do not want wheat flour falling onto your gluten-free pasta.
- Dedicated Equipment: You must have a separate toaster, colander, and wooden spoons. Stainless steel and glass are generally non-porous and can be shared if washed thoroughly, but porous materials like wood and some plastics can harbor gluten.

Mastering Label Reading
In the United States, the FDA’s gluten-free labeling rule is a cornerstone of management. A product labeled “Gluten-Free” must contain less than 20 parts per million (ppm) of gluten. However, reading the ingredient list is still a necessary skill. You must learn to identify hidden sources of gluten such as:
- Malt: Usually derived from barley (e.g., malt vinegar, malt flavoring).
- Brewer’s Yeast: Often a byproduct of beer production.
- Hydrolyzed Wheat Protein: Often found in processed foods and cosmetics.
- Modified Food Starch: Unless specified as corn or tapioca, this can be a risk, though in the US, wheat must be declared.
Social and Emotional Navigation
Perhaps the most complex aspect of celiac disease management is the social component. Food is central to human connection, and dietary restrictions can lead to feelings of isolation or anxiety.
Dining Out Safely
Eating at restaurants requires advocacy and research. It is not enough to ask for a gluten-free menu; you must inquire about kitchen practices. Key questions to ask the server or chef include:
- “Do you have a dedicated fryer for gluten-free items, or is it shared with breaded products?”
- “How do you prevent cross-contact on the grill or prep station?”
- “Is the gluten-free pasta boiled in fresh water or the same water as regular pasta?”
Using apps like ‘Find Me Gluten Free’ can help locate restaurants that are rated highly for celiac safety by the community.

Handling Family Gatherings
Family holidays can be high-stress environments. Well-meaning relatives may not understand the chemistry of cross-contact. Management strategies include bringing your own safe plate, hosting the event yourself to control the kitchen, or having a frank conversation beforehand about safety needs. It is crucial to prioritize your health over social politeness; getting sick is not worth appeasing a relative who insists “one bite won’t hurt.”
Resource Overview
Successful management is easier with the right tools. Building a library of reliable resources ensures you are not navigating this journey alone.
Certification Bodies
Look for third-party certifications on packaging. These organizations often test to stricter standards (such as 10ppm) and inspect manufacturing facilities.
- GFCO (Gluten-Free Certification Organization): Look for the circle with ‘GF’ inside.
- NSF International: Another rigorous testing standard.
- Celiac Support Association: Offers a seal for products testing below 5ppm.
Support Groups
Connecting with local or online support groups can provide emotional validation and practical tips. Organizations like the Celiac Disease Foundation and Beyond Celiac offer extensive educational materials, physician directories, and advocacy updates.
Celiac disease management is a skill that is honed over time. Mistakes will happen, but with a solid “compass” of knowledge regarding adherence, cross-contact, and medical monitoring, you can lead a healthy, symptom-free life. The key is to remain vigilant without letting the disease define your entire existence.
People Also Ask
What is the golden rule of celiac management?
The golden rule is “When in doubt, go without.” If you cannot verify the ingredients or the preparation method of a specific food item, it is safer to skip it than to risk autoimmune damage and symptoms.
Can celiacs eat oats?
Most celiacs can tolerate oats, but they must be certified gluten-free. Regular oats are highly contaminated with wheat during growing and processing. However, a small percentage of celiacs react to avenin, a protein in oats, similar to how they react to gluten.
How long does it take to feel better after starting the diet?
Many patients report feeling better within two weeks of strict gluten elimination. However, complete healing of the intestinal villi can take anywhere from six months to several years, and some symptoms may linger longer than others.
Is sourdough bread safe for celiac disease?
Generally, no. While fermentation breaks down some gluten, traditional wheat sourdough still contains unsafe levels of gluten for celiac patients. Only sourdough made from gluten-free flours (like rice or buckwheat) is safe.
Do I need to change my shampoo and cosmetics?
You should switch to gluten-free versions of any product that might be ingested, such as lipstick, lip balm, toothpaste, and mouthwash. Shampoo and lotion are less critical unless you have a habit of touching your mouth, but many prefer to go 100% gluten-free to reduce risk.
What is refractory celiac disease?
Refractory celiac disease is a rare condition where the intestine fails to heal despite a strict gluten-free diet. It requires specialized medical management, often involving steroids or immunosuppressants, and careful exclusion of other causes for symptoms.
