Coeliac disease is a permanent autoimmune condition where the immune system reacts abnormally to gluten, a protein found in wheat, barley, and rye. In New Zealand, this reaction causes inflammation and damage to the small intestine’s lining, preventing nutrient absorption. It affects approximately 1 in 100 Kiwis and requires a strict, lifelong gluten-free diet for management.
What is Coeliac Disease?
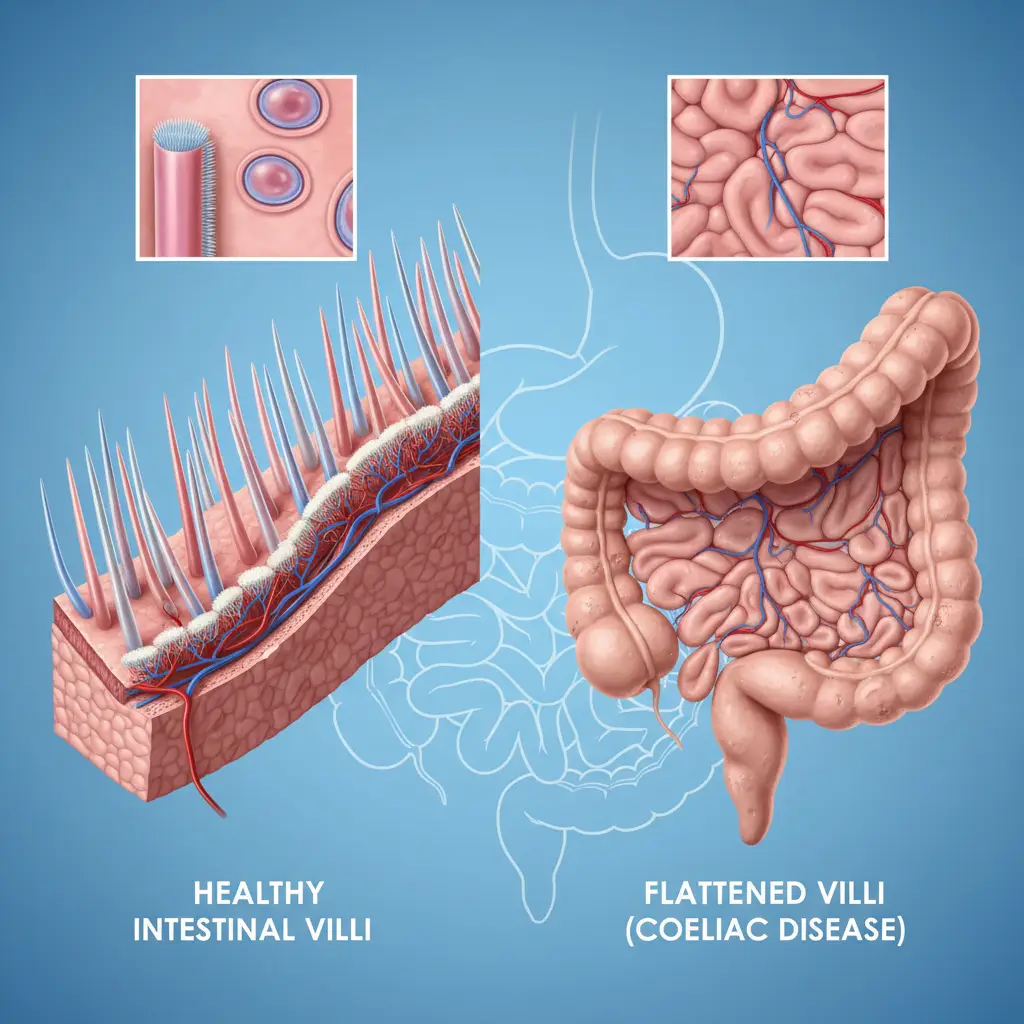
Coeliac disease (spelled Celiac in the United States) is not a food allergy or a dietary intolerance; it is a serious, genetically linked autoimmune disorder. When a person with coeliac disease ingests gluten, their immune system launches an attack against their own body tissues. Specifically, this attack targets the villi—tiny, finger-like projections lining the small intestine responsible for nutrient absorption.
When these villi become inflamed and flattened (a process known as villous atrophy), the surface area available for absorbing nutrients is drastically reduced. Regardless of how much food a person eats, they may become malnourished because vitamins, minerals, and calories essentially pass through the system unabsorbed.
For New Zealanders, understanding this mechanism is crucial because the symptoms are often mistaken for irritable bowel syndrome (IBS) or general stress, leading to delays in diagnosis. Unlike an anaphylactic wheat allergy, the reaction is not always immediate, but the internal damage begins the moment gluten is ingested.
Coeliac Disease Symptoms NZ: Recognizing the Signs
Identifying Coeliac disease symptoms NZ doctors look for can be challenging because the condition is often referred to as a “chameleon.” The symptoms vary significantly from person to person and can manifest at any age, from infancy to senior years. While some Kiwis experience severe gastrointestinal distress, others may have no gut symptoms at all, presenting instead with fatigue or iron deficiency.
Classic Gastrointestinal Symptoms
Historically, coeliac disease was identified by these “classic” symptoms, which remain the most common indicators prompting a visit to a GP in New Zealand:
- Chronic Diarrhoea or Constipation: Persistent bowel irregularity is a red flag.
- Abdominal Pain and Bloating: Severe cramping and a distended stomach, often after meals.
- Nausea and Vomiting: Feeling sick frequently without a viral cause.
- Steatorrhea: Pale, foul-smelling, or fatty stools that are difficult to flush, indicating fat malabsorption.
Non-Gastrointestinal and Systemic Symptoms
In the New Zealand medical context, diagnosis rates are improving as GPs recognize that symptoms often lie outside the gut. These include:
- Unexplained Iron Deficiency Anaemia: This is the single most common symptom of undiagnosed coeliac disease in adults. If you are taking iron supplements but levels remain low, malabsorption due to coeliac disease may be the cause.
- Extreme Fatigue: A deep, unshakeable tiredness (brain fog) that sleep does not cure.
- Dermatitis Herpetiformis: An intensely itchy, blistering skin rash, often on elbows, knees, and buttocks. This is the skin manifestation of coeliac disease.
- Dental Enamel Defects: Discoloration or grooves in teeth, particularly in children.
- Joint and Bone Pain: Unexplained aches or early-onset osteoporosis/osteopenia.
- Fertility Issues: Recurrent miscarriages or unexplained infertility in both men and women.

Silent Coeliac Disease
It is important to note that some individuals have “silent” coeliac disease. They possess the characteristic intestinal damage and positive blood antibodies but report no outward symptoms. These individuals are often diagnosed during screening for other autoimmune conditions (like Type 1 Diabetes or autoimmune thyroid disease) or when a family member is diagnosed. Despite the lack of symptoms, the long-term health risks remain the same if a gluten-free diet is not adopted.
Prevalence in New Zealand
According to Coeliac New Zealand, the condition affects at least 1 in 100 New Zealanders. However, it is estimated that up to 80% of those with the condition remain undiagnosed. With a population of over 5 million, this means there are likely between 60,000 to 100,000 Kiwis living with the disease, many unknowingly.
The prevalence is higher in individuals who have a first-degree relative (parent, child, sibling) with coeliac disease, with the risk jumping to approximately 1 in 10. Consequently, if one family member in a Kiwi household is diagnosed, it is strongly recommended that all immediate family members be screened, regardless of whether they display symptoms.
The Diagnosis Pathway in Aotearoa
If you suspect you have coeliac disease, it is critical that you do not stop eating gluten before testing. Removing gluten from your diet before medical testing can lead to a false-negative result, as the body heals and antibodies drop.
Step 1: Coeliac Serology (Blood Test)
The first step is a simple blood test arranged by your General Practitioner. This test looks for specific antibodies, primarily Tissue Transglutaminase antibodies (tTG-IgA). In New Zealand, this initial screening is generally funded for eligible residents.
Step 2: Gastroscopy and Biopsy
If the blood test is positive, you will typically be referred to a gastroenterologist for a gastroscopy. This procedure involves passing a thin, flexible tube with a camera down the throat to examine the small intestine. Small tissue samples (biopsies) are taken to check for villous atrophy. This is the “gold standard” for diagnosis in New Zealand.
While waiting for these appointments (which can take time in the public health system), you must continue consuming a normal diet containing gluten (equivalent to four slices of bread daily) for at least six weeks prior to the procedure to ensure accuracy.

Understanding NZ Gluten-Free Standards
One of the most distinct aspects of managing coeliac disease in New Zealand is our food labeling laws, which are among the strictest in the world. Governed by Food Standards Australia New Zealand (FSANZ), the definition of “Gluten-Free” here differs from the USA and Europe.
No Detectable Gluten vs. 20ppm
In many parts of the world (including the UK, EU, and USA), a product can be labeled “Gluten-Free” if it contains less than 20 parts per million (ppm) of gluten. However, under the FSANZ code used in New Zealand:
- Gluten-Free: The product must contain no detectable gluten using the most sensitive commercial testing methods available. It must also not contain oats or malted cereals.
- Low Gluten: This is a separate category for products with less than 200ppm (but detectable gluten). This category is generally not recommended for people with coeliac disease.
This strict standard provides an extra layer of safety for Kiwi coeliacs. When shopping at local supermarkets like Countdown, New World, or Pak’nSave, looking for the “Gluten Free” label or the Coeliac New Zealand “Crossed Grain” logo ensures the product meets these rigorous standards.
Living the Gluten-Free Lifestyle in NZ
Managing coeliac disease requires a complete lifestyle overhaul. In New Zealand, this is becoming easier due to increased awareness, but cross-contamination remains a significant risk.
Navigating “May Contain” Statements
In New Zealand, allergen labeling is mandatory. You must learn to read the back of the pack, not just the front. Manufacturers must declare if wheat, rye, barley, or oats are present as ingredients. Precautionary statements like “May contain traces of gluten” are voluntary but should be heeded by those with coeliac disease, as they indicate a risk of cross-contamination during manufacturing.
Dining Out in Aotearoa
Eating out is a major part of Kiwi culture, from cafe brunches to fish and chips. However, deep fryers are a common source of cross-contamination. If a takeaway shop cooks gluten-free chips in the same oil as battered fish or crumbed sausages, those chips are not safe for a coeliac.
Coeliac New Zealand offers a “Dining Out Programme” which accredits venues that follow strict gluten-free preparation protocols. Seeking out these accredited venues is the safest way to enjoy a meal out.

Support and Subsidy
Living gluten-free can be expensive. In New Zealand, Pharmac (the government pharmaceutical buying agency) provides a subsidy for gluten-free staple foods (like flour and baking mixes) for diagnosed coeliacs. To access this, you need a biopsy-confirmed diagnosis and a prescription from your GP or specialist. This “Special Authority” allows you to collect monthly supplies from your pharmacy, significantly offsetting the grocery bill.
Frequently Asked Questions
Is Coeliac disease considered a disability in NZ?
While Coeliac disease is a serious medical condition, it is not typically classified as a disability in New Zealand for the purpose of receiving a disability allowance, unless the complications are severe and disabling. However, the Pharmac subsidy for food helps offset the cost of treatment (the diet).
Can you grow out of Coeliac disease?
No, Coeliac disease is a lifelong autoimmune condition. It is not a childhood phase. Once diagnosed, you must adhere to a gluten-free diet for the rest of your life to prevent damage to your body.
What is the difference between gluten intolerance and Coeliac disease?
Coeliac disease involves the immune system damaging the intestine and can lead to long-term health issues like osteoporosis and cancer. Non-Coeliac Gluten Sensitivity (intolerance) may cause similar symptoms but does not cause damage to the intestine or trigger the autoimmune response.
Are oats gluten-free in New Zealand?
Under current FSANZ laws, oats cannot be labeled “Gluten-Free” in New Zealand. This is because a protein in oats called avenin mimics gluten and causes a reaction in approximately 20% of coeliacs. Furthermore, oats are often cross-contaminated with wheat during processing.
How long does it take for gut villi to heal?
For most people, symptoms improve within weeks of starting a gluten-free diet. However, the villi in the small intestine can take anywhere from six months to two years to fully heal, depending on the severity of the damage and strict adherence to the diet.
Does a blood test confirm Coeliac disease 100%?
No. While modern serology tests are highly accurate, they are not definitive. A positive blood test indicates a high probability, but a gastroscopy with a biopsy is required to confirm the diagnosis and assess the extent of the damage to the intestine.
